Gastric Sleeve Surgery
Gastric sleeve surgery, also known as sleeve gastrectomy, is a surgical procedure that aims to aid weight loss in individuals with obesity. It involves the removal of a large portion of the stomach to create a smaller, sleeve-shaped stomach. This reduction in stomach size helps limit food intake and promotes a feeling of fullness, leading to weight loss.
Here is a detailed summary of the gastric sleeve operation:
1. Pre-operative preparation: Before the surgery, there will be an evaluation by healthcare team, which may include a physical examination, blood tests, imaging studies, and consultations with a nutritionist or dietitian. This assessment helps determine your eligibility for the surgery and ensures you are adequately prepared for the procedure.
2. Anesthesia: On the day of surgery, you will be administered general anesthesia, which will keep you unconscious and pain-free during the procedure.
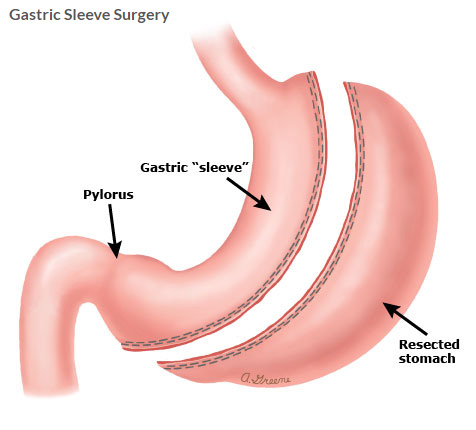
3. Surgical procedure: The gastric sleeve surgery is typically performed using minimally invasive laparoscopic techniques. Several small incisions are made in the abdomen, through which surgical instruments and a laparoscope (a thin tube with a camera) are inserted. The surgeon then proceeds with the following steps:
a. Stomach Reduction: The surgeon removes approximately 70-80% of the stomach, leaving behind a smaller, tube-shaped stomach or "sleeve." The remaining stomach is sealed using surgical staples or sutures.
b. Reinforcement: In some cases, the surgeon may reinforce the staple line with additional sutures or use a buttressing material to reduce the risk of leaks or complications.
4. Post-operative care: After the surgery, you will likely experience some pain, which can be managed with pain medications. In the initial days following surgery, you will receive clear fluids, and gradually transition to a pureed and then solid food diet under the guidance of a dietitian.
5. Hospital stay and follow-up: The length of hospital stay varies but is typically around 2-3 days, depending on your overall health and recovery progress. During your hospital stay, the healthcare team will guide your vital signs, manage pain, supply medications, and provide instructions on post-operative care.
6. Recovery and lifestyle changes: After discharge, you will need to make significant lifestyle changes to support your weight loss and overall health. This includes following a strict dietary plan, engaging in regular physical activity, and attending regular follow-up appointments with your healthcare team for monitoring and support. Dietary guidelines will focus on consuming small, nutrient-dense meals and avoiding high-calorie and sugary foods.
7. Weight loss and long-term outcomes: Gastric sleeve surgery typically results in significant weight loss over time. Most individuals experience the most rapid weight loss in the first 12-18 months following surgery, with continued progress over the next several years. The amount of weight loss varies among individuals, but it is common to see a loss of 50-70% of excess body weight within the first two years after surgery.
It's important to note that gastric sleeve surgery is a major surgical procedure that carries risks and requires careful consideration. It should only be pursued after thorough evaluation and discussions with your healthcare team. The procedure can provide significant benefits in terms of weight loss and improvement in obesity-related conditions, but long-term success requires adherence to lifestyle changes and ongoing support from a healthcare team.
Who are suitable for Gastric Sleeve Surgery?
Gastric sleeve surgery is typically recommended for individuals who meet certain criteria and have been unable to achieve sustainable weight loss through non-surgical methods such as diet and exercise. While each case is unique and should be evaluated by a healthcare professional, here are general guidelines for individuals who may be considered suitable candidates for gastric sleeve surgery:
- Body mass index (BMI): Gastric sleeve surgery is typically recommended for individuals with a BMI of 40 or higher (severe obesity) or a BMI of 35-39.9 (obesity) with obesity-related health conditions such as diabetes, high blood pressure, or sleep apnea. However, the specific BMI cutoffs may vary based on individual circumstances and regional guidelines.
- Failed attempts at non-surgical weight loss: Candidates for gastric sleeve surgery should have made previous attempts at weight loss through diet, exercise, and other non-surgical interventions without achieving significant and sustainable results.
- Absence of medical contraindications: Candidates should be in overall good health and free from medical conditions that may pose excessive risks during surgery or the recovery period. Common contraindications may include severe heart or lung disease, bleeding disorders, uncontrolled psychiatric conditions, or active substance abuse.
- Psychological evaluation: Candidates typically undergo a psychological evaluation to assess their readiness for the surgery and their ability to cope with the emotional and psychological changes that may accompany significant weight loss.
- Age considerations: Age alone does not disqualify someone from gastric sleeve surgery. However, the procedure is generally recommended for individuals who have reached skeletal maturity, which is typically around the age of 18. Exceptions may be made for adolescents who have severe obesity and obesity-related health complications.
It's important to note that these criteria serve as general guidelines, and the final decision regarding candidacy for gastric sleeve surgery should be made after a comprehensive evaluation by a qualified healthcare professional. They will assess your individual health status, weight history, lifestyle factors, and specific goals to determine the most appropriate treatment options for your unique situation.
What are the complications that may occur in gastric sleeve surgery?
What are the precautions?
Gastric sleeve surgery, like any surgical procedure, carries risks and potential complications. It's essential to be aware of these risks and take necessary precautions to minimize them. Here are some possible complications associated with gastric sleeve surgery:
- Infection: There is a risk of infection at the incision sites or within the abdominal cavity. Precautions include sterile surgical techniques, proper wound care, and the appropriate use of antibiotics.
- Bleeding: Bleeding can occur during or after the surgery. The surgical team takes precautions to control bleeding during the procedure. In some cases, additional interventions may be required to address excessive bleeding.
- Leaks: Leakage of stomach contents from the staple line can occur, leading to infection or other complications. Precautions such as proper technique and reinforcement of the staple line are taken to minimize the risk of leaks. Monitoring for signs of leakage post-surgery and prompt intervention if detected is crucial.
- Strictures: Narrowing or tightening of the remaining stomach (stomal stenosis) can occur, making it difficult to pass food through. Regular follow-up appointments and appropriate dietary modifications can help detect and manage strictures.
- Gastroesophageal reflux disease (GERD): Some individuals may experience increased acid reflux or heartburn symptoms after surgery. Precautions include pre-operative evaluation and appropriate management of pre-existing GERD, as well as post-operative dietary and lifestyle modifications to minimize symptoms.
- Nutritional deficiencies: After gastric sleeve surgery, individuals may be at risk of nutrient deficiencies due to reduced food intake and malabsorption. Precautions involve close monitoring of nutritional status, regular follow-up with a dietitian, and adherence to prescribed vitamin and mineral supplementation regimens.
- Dumping syndrome: Rapid emptying of stomach contents into the small intestine can cause symptoms such as nausea, weakness, sweating, and diarrhea. Precautions involve eating small, frequent meals, avoiding high-sugar or high-fat foods, and properly chewing food to minimize the risk of dumping syndrome.
It's important to note that complications are relatively rare, and the majority of gastric sleeve surgeries are successful with favorable outcomes. However, it is crucial to choose an experienced surgeon and follow all pre-operative and post-operative instructions carefully to reduce the risks associated with the procedure. Regular follow-up appointments and open communication with your healthcare team are vital for monitoring your progress, addressing any concerns promptly, and ensuring a successful recovery.
